Interoperability between health IT systems is one of the biggest challenges facing healthcare systems and their IT specialists, as the seamless and secure flow of data from one place to another is critical for improving patient outcomes across disparate departments and providers. According to the 21st Century Cures Act, interoperability is defined as healthcare technology that enables the secure exchange of electronic health information using health information from other health IT without special effort on the part of the user; allows for complete access, exchange, and use of all electronically available health information; and does not constitute information blocking, as defined by the law.
Per today’s laws, such data must be both transmitted and written in ways that make it possible to move data from one electronic health record (EHR) system to another, making it easier for healthcare providers to understand the full picture of a patient’s medical history without having to jump through hurdles and, instead, placing the burden on the patient to provide that critical information.
There are four levels of interoperability, according to the Healthcare Information and Management Systems Society (HIMSS):
- Foundational (Level 1): Establishes the inter-connectivity requirements needed for one system or application to securely communicate data to, and receive data from, another
- Structural (Level 2): Defines the format, syntax, and organization of data exchange, including at the data field level for interpretation
- Semantic (Level 3): Provides for common underlying models and codification of the data, including the use of data elements with standardized definitions from publicly available value sets and coding vocabularies, providing shared understanding and meaning to the user
- Organizational (Level 4): Includes governance, policy, social, legal, and organizational considerations to facilitate the secure, seamless and timely communication and use of data, both within and between organizations, entities, and individuals. These components enable shared consent, trust, and integrated end-user processes and workflows.
While the ultimate goal of achieving interoperability is to give providers the most comprehensive view of a patient’s health needs as possible, comprehensive data sharing is also key for healthcare organizations hoping to earn incentive payments through the Centers for Medicare and Medicaid Services (CMS) Promoting Interoperability Program.
In 2020, CMS published the CMS Interoperability and Patient Access Final Rule, which established policies that advance interoperability and access to health data for all stakeholders, including patients, with the rule is designed to make sure patients have convenient access to their healthcare data through a personal health app.
In addition, the rule requires certain payers to build standardized application programming interfaces to allow for the exchange of information with other payers, with the goal of enabling patients’ health data to follow them, if they switch health insurance plans.
In short, the U.S. healthcare industry has no choice but to comply with the provisions in the Cures Act; however, legacy integration tools don’t provide a seamless, scalable, and centralized platform with APIs that enable healthcare IT vendors, medical billing organizations, and digital health companies to overcome interoperability challenges and manage their data integration hurdles.
The ultimate goal of healthcare technology interoperability is to break down the silos that exist between disparate healthcare IT products and facilitate access to clinical data, which helps healthcare professionals provide effective and equitable patient-centered care, as well as provide actionable data to health agencies.
Challenges of interoperability
However, despite those federal initiatives, many challenges remain, including a lack of system integrations, the disjointed enforcement of health IT interoperability standards across settings, difficulty enforcing industry-wide interoperability measurement standards, coordinating stakeholders across the industry, and information blocking. The benefits of interoperability are clear, with healthcare leaders clamoring for the industry to adapt to these challenges. There are hundreds of government-certified EHR products on the market, each with their own clinical terminologies, technical specifications, and capabilities. Those differences make it difficult to create one standard interoperability format for sharing data across organizations and medical software. Even EHR systems built on the same platform may not be interoperable, since they are usually customized to an organization’s needs.
While technological challenges are apparent, cultural challenges also present a big obstacle facing healthcare IT interoperability, as the U.S. healthcare system is built on a culture of siloed and fragmented systems and disparate stakeholders.
Benefits of interoperability
Throughout a patient’s time in the healthcare system, they receive treatment from a variety of sources, including clinic, independent practices, hospitals, and other providers. The records from each source are critical for the patient’s next provider to access. Without access to information on the patient’s medical history, providers could make crucial mistakes. At the very least, the lack of interoperability is inconvenient for the patient, who is then tasked with coordinating medical records transmission. Interoperability also streamlines a provider’s access to real-time medical records and cuts down on administrative tasks, enabling providers to improve their quality of care and treat more patients. Patients will have more control over their own data, removing a significant amount of that administrative burden. The remaining administrative and clinical functions will be streamlined due to accurate data and insights.
As mentioned before, healthcare organizations have every incentive to help enable data sharing, as they could become eligible for incentive payments through the Centers for Medicare and Medicaid Services (CMS) Promoting Interoperability Program.
Interoperability essentially enhances the experience for all stakeholders, so healthcare groups are all-in on investing in interoperability, with clear benefits not only to clinical care, but also to help providers understand costs, utilization, and populations.
Integrations between healthcare software have never been more important, and it is becoming critical that organizations are able to easily and seamlessly transmit and receive health data.
CareCloud Connector can help break down those silos
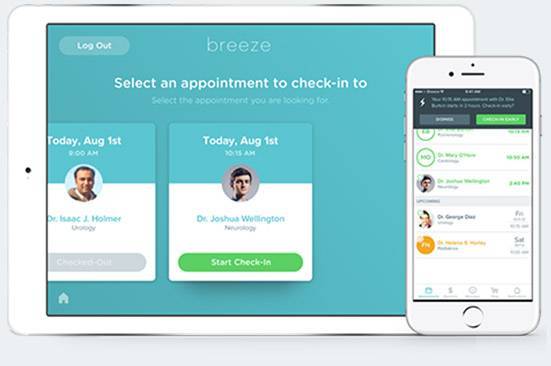
In response to these challenges, CareCloud recently released CareCloud Connector (Connector), a next-generation interface and data management engine that provides healthcare organizations with ready-to-use integrations that improve data management and deployment speed, while offering better interface visibility and control.
The platform provides organizations with the same turn-key integration technology and tools used by CareCloud to manage health organizations across hundreds of unique integrations spanning thousands of locations.
CareCloud Connector provides a seamless, scalable, and centralized platform with APIs, allowing healthcare IT vendors, medical billing organizations, and digital health companies to overcome interoperability challenges and effectively manage data integration and transmission hurdles. Connector includes a library of industry-tested, ready-to-use integrations, interfaces, and customizable tools in a convenient SaaS offering.
CareCloud Connector is one of the healthcare industry’s first true libraries of plug-and-play integration and customizable tools, helping to inject simplicity and security into typically time-consuming developmental projects. With Connector, the industry can close interoperability gaps, while helping health organizations and service providers save time and money.
In fact, Connector is the first solution launched under the new CareCloud Conductor (Conductor) suite, a new family of technologies designed to support interoperability, connectivity, and data transformation.
Stay tuned for more Conductor product announcements this year, as we look forward to supporting the growing prominence of health IT developers and investments in digital health.